“Two Powerful Drugs Now Adding to U.S. Overdose Crisis,” reported the Associated Press in a January 27 story.
“Emerging reports show that two little-known drugs are making lethal new contributions to America’s drug overdose crisis.
“Para-fluorofentanyl and metonitazene are being seen more often by medical examiners looking into overdose deaths. They often are taken with — or mixed with — illicit fentanyl, the drug mainly responsible for the more than 100,000 U.S. overdose deaths in the last year.”
Dr. Darinka Mileusnic-Polchan, one of the report authors, said the drugs are injected or snorted and are more powerful than fentanyl.
“‘These (victims) just crumple and collapse. Frequently they don’t even inject the full syringe before overdosing,’ said Mileusnic-Polchan, who leads the medical examiner’s office in Knoxville, Tennessee.”
At the Pacific Palisades Task Force on Homelessness quarterly meeting on January 24 on Zoom, Dr. Christine Grella, the co-director of UCLA’s Integrated Substance Abuse Programs, spoke on “The Hope and Challenges of Treating Addiction.”
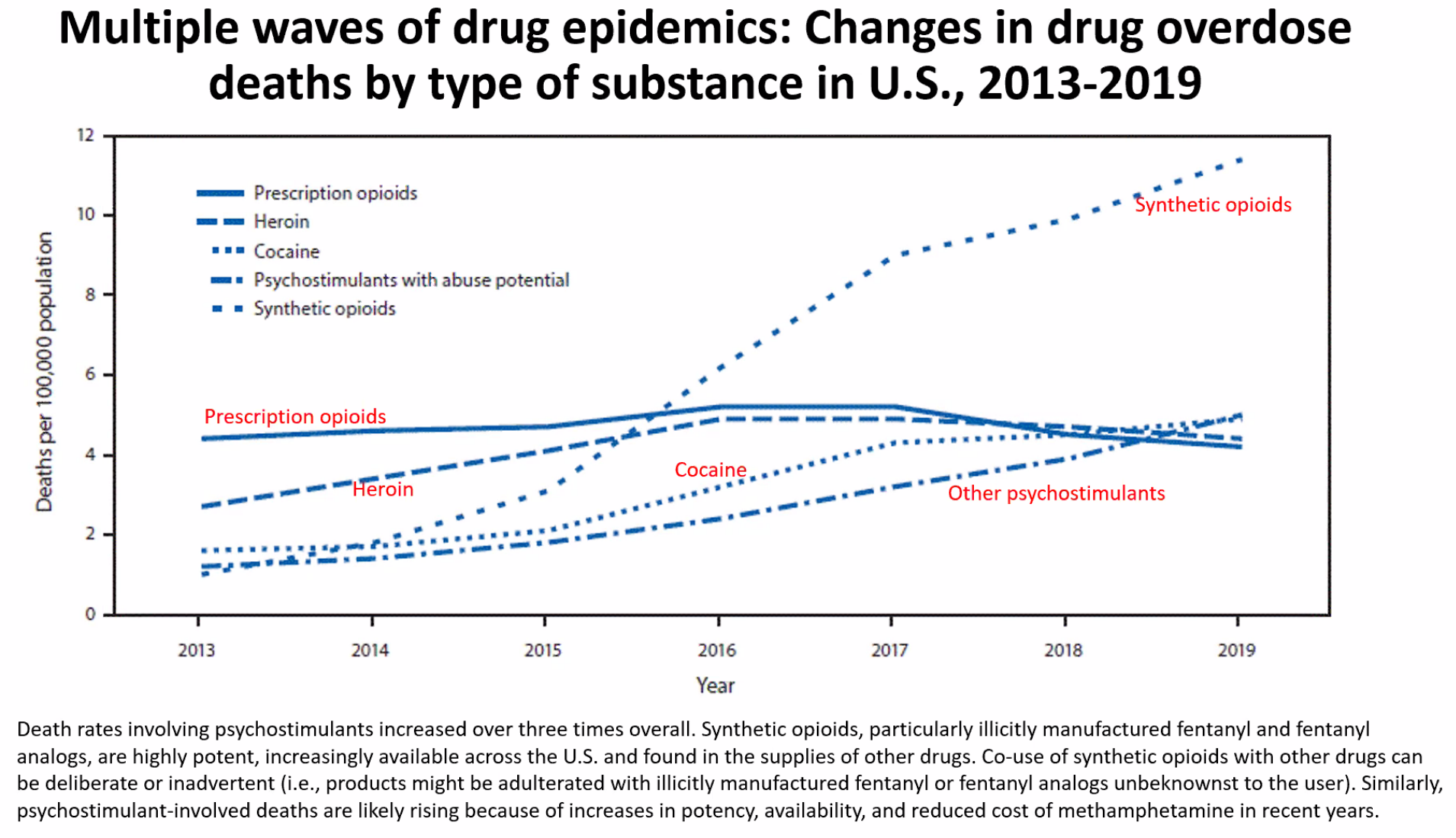
Grella said that overdose deaths by synthetic opioids had increased by three times from 2013 to 2019.
“The deaths are likely rising because of the increases in potency, availability and reduced cost of methamphetamine in recent years,” she said, noting that drug overdose is the leading cause of death among people experiencing homelessness in L.A. County.
From 2018 through July 2020, meth has been the leading cause of overdoses. Deaths attributed to fentanyl started to rise dramatically from 2019 through 2020.
Meth is a powerful, highly addictive stimulant that affects the central nervous system and can be smoked, inhaled, injected or orally ingested. The risk of overdose is heightened when combined with other substances, such as opioids, synthetics such as fentanyl, alcohol and sedatives.
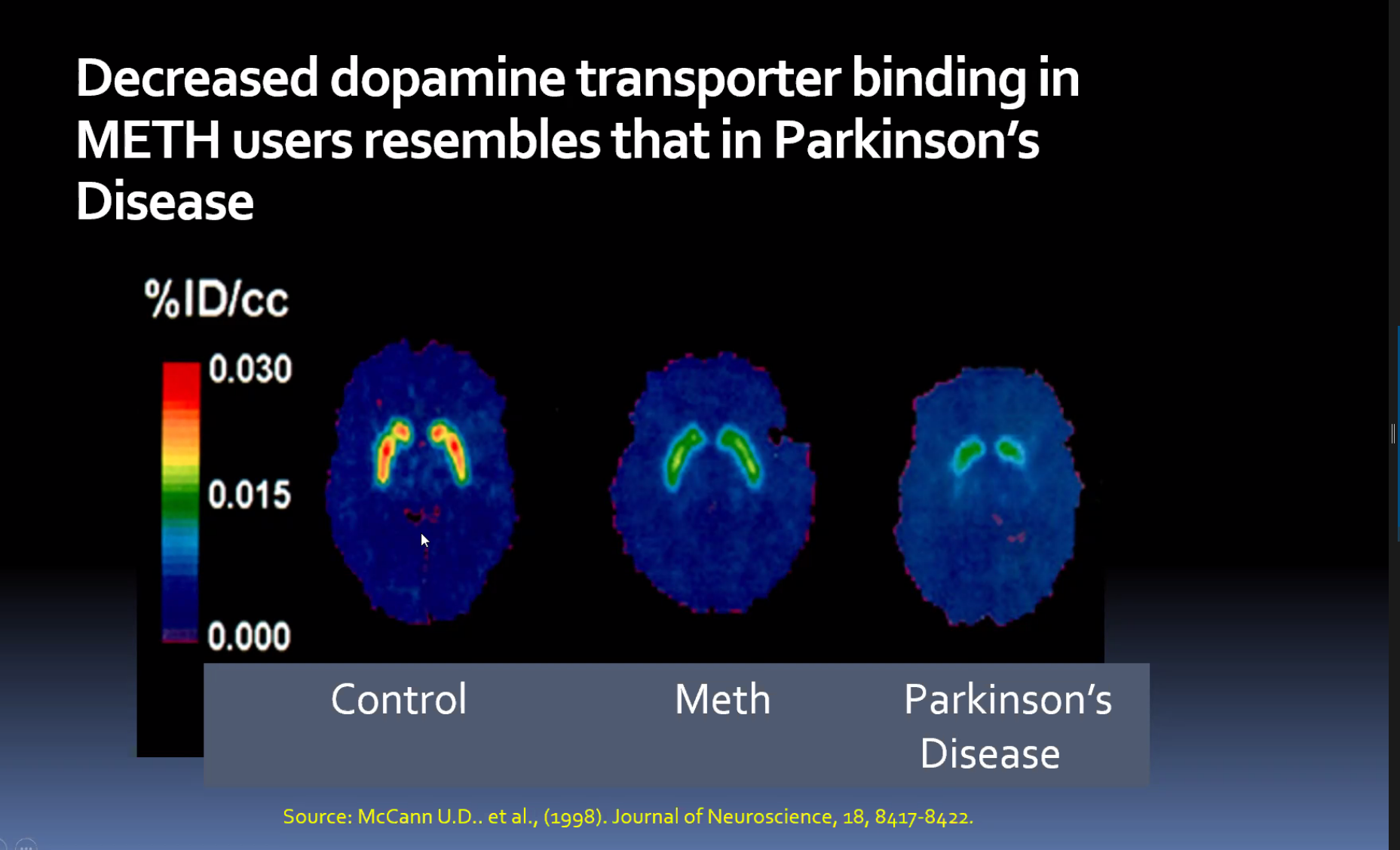
Taking meth over time results in the image of a brain looking like that of a person who has Parkinson’s disease. Although a disease is generally defined by a biological disorder, addiction, has been likened to a disease.
The study of biochemistry and those who become addicted is summarized in “The Neurobiology of Addiction: Where We Have Been and Where We Are Going” (2009 – NCBI https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2901107/) as “the big disappointment to scientists in this field is that 34 years into the modern era of drug abuse research, we still do not have a clear understanding of the cellular and molecular bases of the development and maintenance of the phenomena of addiction, such as tolerance, physical dependence, and psychic craving.”
What options are there for those who have substance abuse? There is not a magical cure, and Grella said that service providers have few options for people who are using but do not want to go into treatment.
The United States population has a large number of people who struggle with addictions/alcoholism.
Grella said that 9.1 percent of U.S. adults surveyed said they “used to have a problem with drugs or alcohol, but no longer do” and about half of those identified are in recovery.
There are currently three methods used for treatment: Clinical pathways, which includes self-help programs; non-clinical pathways, which are community based, such as sober dorms and peer support; and self-management (natural recovery).
Grella spoke about the need to take away the stigma of addiction and to decriminalize the actions.
When a meeting participant asked about just putting people in jail, so they can get “clean,” she responded: “The treatment system in jails is poorly implemented,” and the overdose rate is extremely high for those that are released after being incarcerated.
Grella said that the drug-court models, when addicts are required to go into treatment under judges’ orders, “have worked really well.” She also said that the peer recovery models are “incredibly powerful and effective.”
She was asked about the homeless people she sees on the streets who have mental issues, drug issues or both.
“When we see people who are very ill, such as from cancer, we would say, this person needs help,” Grella said. “But when we see people with mental health or substance issues, we don’t do anything.”
Visit: pptfh.org.