Who would have thought by stating a fact that obesity is a major factor in Type 2 diabetes, coronary heart disease, gallbladder disease, sleep apnea and respiratory
problems and some cancers — and Covid-19 — that it would be considered a political issue?
According to research conducted by the Harvard T.H. Chan School of Public Health, it is estimated that in 2019 about 40 percent of Americans were considered obese, and
18 percent were considered severely obese.
Too many Americans are fat. No nice way to put this or to “sugar-coat” what the research shows.
Globally, it might seem that the U.S. is in the lead, but we are only the 12th most obese country, behind Nauru, Cook Islands, Palau, Marshall Islands, Tuvalu, Niue, Tonga, Samoa, Kiribati, Micronesia and Kuwait. By comparison, Canada is 26 and Mexico is 28.
Strictly from a statistical point, non-Hispanic Asian adults have the lowest rates of obesity and non-Hispanic Black adults have the highest rate.
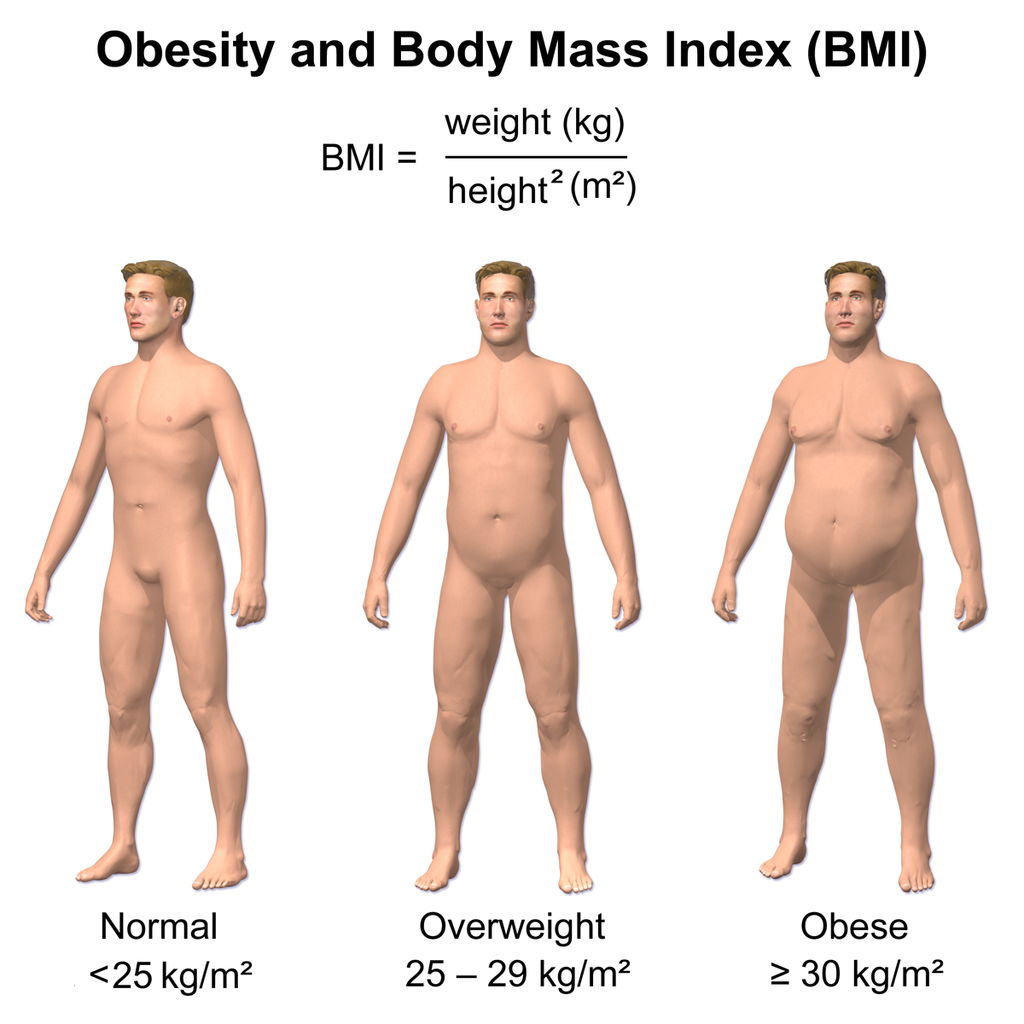
Obesity in adults is defined as a Body Mass Index of greater than or equal to 30 and severe obesity as a BMI of greater than or equal to 40.
To find your BMI, take your weight in kilograms divided by height in meters squared, rounded to one decimal place. I weigh 144 pounds, so if one pound equals 0.454 kilogram, then I am 65.3 kg. Next, I’m 5’9″ (divide the length value by 3.281, once again that converts to 1.753 meters and squared is 3.07.) So I have a BMI of TK. Or just visit: https://www.nhlbi.nih.gov/health/educational/lose wt/BMI/bmicalc.htm.
BMI Categories:
Underweight = <18.5
Normal weight = 18.5-24.9
Overweight = 25-29.9
Obesity = BMI of 30 or greater
 Why can’t obesity be a health topic addressed like smoking? Chances are if you are an adult and you chose to smoke, your life expectancy is shorter. The same is true of obesity.
Why can’t obesity be a health topic addressed like smoking? Chances are if you are an adult and you chose to smoke, your life expectancy is shorter. The same is true of obesity.
 A 2018 Australian study, published in the International Journal of Obesity, showed that young adults classified as obese could expect to lose up to 10 years in life expectancy.
A 2018 Australian study, published in the International Journal of Obesity, showed that young adults classified as obese could expect to lose up to 10 years in life expectancy.
Lead author Dr. Thomas Lung, from The George Institute for Global Health, said the most alarming findings where those among people in their 20s and 30s.
“We know that excess weight has an impact on your health, but to have excess weight as a young adult is really significant on life expectancy. We are talking about losing up to 10 years of your life,” said Dr. Lung.
“The model predicted remaining life expectancy for people in their 20s, 30s, 40, 50s and 60s in healthy, overweight, obese and severely obese weight categories. It also calculated the number of years lost over the lifetime for people with excess weight in each age group, compared to those with a healthy weight.
When Circling the News observed in April that Covid-19 was particularly dangerous for those considered obese, and spoke to a person in the State of California Department of Public Health, asking why instead of trying to tie the disease to melanin (skin color), why not warn people that severe Covid-19 outcome is related to obesity? CTN was ignored.
The Centers for Disease Control reported that “Having obesity may triple the risk of hospitalization due to a Covid-19 infection. Obesity is linked to impaired immune function. Obesity decreases lung capacity and reserve and can make ventilation more difficult. As BMI increases, the risk of death from Covid-19 increases.”
The growing obesity in this country—across all racial lines — is certainly not new. Back in 2012, Harvard Men’s Health Watch (“Obesity in America: What’s Driving the Epidemic?”) wrote, “In some cases, genetics seem responsible; in others, various combinations of hormonal, metabolic, and behavioral factors appear to play a role. But in most cases, it’s hard to determine the exact cause of obesity.”
The story noted that in less than 40 years, the prevalence of obesity in the United States had increased by more than 50%, so that two of every three American adults were now overweight or obese.
Why has America become more obese? According to the report, lack of exercise and the increase in calories.
According to the U.S. Bureau of Labor Statistics, “Researchers evaluated the relationship between physical activity in the workplace and obesity over the past several decades. In 1960, nearly half the jobs in the private sector required at least moderate physical activity, but in 2010, less than 20% demanded this much physical work . . ..means that the average American man is now burning 142 fewer calories each day than he did in the 1960s.”
From 1960 to 1962, the average American man weighed 169 pounds, but between 2003-2006, he weighed 202 pounds.
The study pointed out that the actual percentage of adults who get enough leisure-time exercise is about five percent. Leisure-time exercise is defined as walking for 30 minutes a day.
Americans spend too much time sitting—particularly now with gyms and schools closed and meetings online.
An American Cancer Society (ACS) study of 123,216 adults with an average age of 63 found that the death rate of men who spent the most time sitting was 17% higher than that of their peers who spent the least time sitting (even adjusted after cardiovascular risk factors were taken into account).
A 2011 European seven-year study that focused specifically on TV watching reported similar results. “The men who spent the most time watching TV (an average of over 3.6 hours a day) were compared with the men who spent the least time (less than 2.5 hours a day) in front of the tube.
Even though the heavy-duty TV watchers did not consume more calories than the other men, they ate fewer fruits and vegetables and had larger waistlines and higher levels of blood pressure, blood sugar, and triglycerides, as well as lower levels of HDL (“good”) cholesterol.”
The study reported that each hour of TV viewing per day was linked to an increase in diabetes, heart disease and a higher death rate. (These studies were done before computers, laptops and iPhone screen time were factored into the amount of time one sits—and anecdotally that time has skyrocketed.)
Snacks, unhealthy and processed food and portion-size have also been blamed for the obesity epidemic. The University of North Carolina evaluated data from four large national surveys that included 44,754 Americans ages 19 and above from 1977 to 2006.
Weight gain was linked to a high intake of potato chips, potatoes, sugar-sweetened beverages, red meat, and processed meat. In contrast, a high intake of vegetables, whole grains, fruits, nuts, and yogurt appeared to protect against gaining weight.
“Although the caloric content of individual meals and snacks stabilized, Americans began eating more often. Over the 30-year period, the average number of meals and snacks rose from 3.8 a day to 4.9 a day.”
Sleep was also important in weight gain. Sleeping too little (less than six hours a day) or too much (over eight hours a day) predicted the greatest weight gain.
Alcohol? Generally moderate drinking (up to two drinks a day for men) appears to reduce the risk of heart attack and stroke. But alcohol is a calorie-dense food and one drink a day provides enough calories to pack on 10 pounds over the course of a year.
People know that they should eat the right foods, eat less and exercise. Why isn’t that happening?
According to the Harvard report, “The food and entertainment industries push back with seductive ads that trump somber warnings. And as people get fatter, they slowly accept corpulence as the new normal and then spread their apparent embrace of extra pounds to friends and neighbors through social networks.”
It seems that obesity should get new attention as a health problem such as smoking. Politics need to be taken out of it.
In a 2012 “Everday Health” story (“Is Promoting Big Beautiful Woman
Unhealthy?”) Susan Levin, MS, RD, and director of nutrition education at the Physicians Committee for Responsible Medicine, wrote, “The list of risks that come with being overweight or obese is quite extensive and incredibly serious. What we’re talking about here is not just physical appearance.
“We want to celebrate how everyone looks and never want to make someone feel bad about the way they look. But being overweight or obese isn’t something that is handed to you that you have no control over.”
Circling the News was sent “Fat Shaming Won’t Solve Obesity. Science Might.” (labblog.uofmhealth.org), which was a roundup of 15 research papers from “Michigan Medicine” that proved the treatment for obesity can’t adopt a “one size fits all” approach.
The papers can be divided into:
1) Economic, such as “Low-Income Communities More Likely to Face Childhood Obesity,” which notes that “access to recreational programs and full service grocery stores appears to have a greater impact on the nation’s childhood obesity rate than race.”
2) Brain chemistry: (“Resisting Food Temptation Isn’t Futile, but Obesity May Make it Harder”), which states some of us are powerless to resist temptation, and “Clues to Obesity Roots Found in Brain’s Quality Control Process” and “Does Gut Bacteria Lead to Obesity?” 3) Self-determination, such as “Chronic Short Sleep Associated with Adolescent Obesity” to “Fitness Vs. Fatness: Which Matters Most?”
Americans are getting fatter and people need to know with excess weight gain, they will not live as long as their grandparents. Obesity is associated with health conditions.
Much like smoking, if an individual knows the health risks of being overweight and accepts it, that is his/her choice.
But this is not a political issue of whether someone is beautiful, or not, because they are overweight. This is not about fat-shaming, this is about choices and health consequences associated with those choices.